Neurosurgeons at Penn Medicine are performing unilateral MR image-guided focused ultrasound (MRgFUS) thalamotomy for patients with essential tremor (ET) refractory to medication. First FDA-approved for unilateral application in medically-intractable patients with ET as an alternative to thalamotomy and DBS, MRgFUS received a second indication in 2021 as a supplement to medication treatment for unilateral pallidotomy in medication-resistant Parkinson's disease patients with moderate to severe motor complications. In December 2022, MRgFUS received a third indication (and second in ET) for staged, bilateral treatment of medication-refractory essential tremor, permitting contralateral treatment at least nine months after initial therapy in patients with bilateral tremors from ET. Penn Neurosurgery was among the sites for the study submitted to the FDA for this indication. MRgFUS has been available at Penn Neurosurgery since 2017.
Essential Tremor Disorder - Symptoms and Causes
ET is a progressive neurologic disorder characterized by rhythmic, involuntary postural and intention (action) tremors. It is not associated with Parkinson's disease. The upper limbs are affected in ~95% of patients with ET, with substantial population subsets having head and lower limb tremor. Although not fatal, ET can cause considerable disability and quality of life detriments as the amplitude of tremor increases over time. Some sources now include non-motor effects in the constellation of ET, including cognitive impairment and psychological issues. While the exact origin of ET is unknown, post-mortem reports implicate structural changes in the cerebellum in the condition's pathophysiology; other studies have identified single-unit tremor-related discharges coherent with tremor (e.g., tremor cells) in the ventral intermediate nucleus (VIM) of the thalamus in ET and PD patients.
Traditional and Novel Treatments for ET
The first-line treatments for ET include propranolol and primidone. Adverse effects and insufficient efficacy are impediments to these agents, and many patients become medication-refractory over time. Safe and efficacious therapies are available for medically intractable ET, but here again there are concerns in that many patients do not wish to have invasive procedures involving the brain. Of the approved treatments — thalamotomy, deep brain stimulation (DBS), and MR-guided focused ultrasound (MRgFUS) — only the latter is noninvasive.
About MR Image-Guided Focused Ultrasound
MRgFUS combines MR imaging with ultrasound beam technology to first target and then ablate cells involved in the emergence of tremor in the ventral intermediate nucleus of the thalamus. At this time, MRgFUS is indicated for unilateral thalamotomy and staged bilateral procedures with the treatment of the second side at least 9 months later.
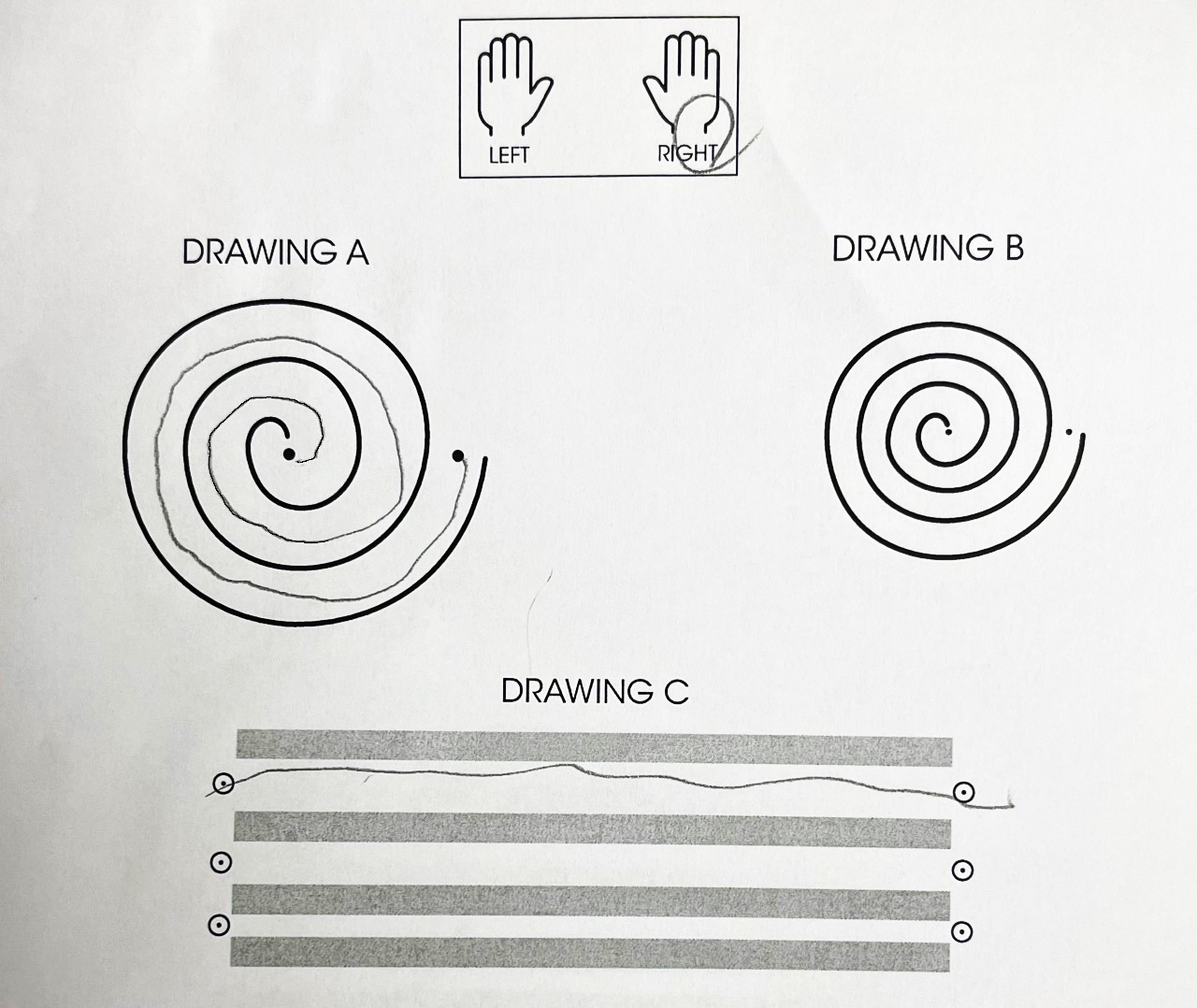
The Procedure: MRgFUS thalamotomy involves the real-time interaction of a neurosurgeon and patient, who is awake and responsive throughout the procedure. Prior to MRgFUS, the patient may be asked to draw a spiral to determine the effectiveness of the therapy afterward (Figure 1). The patient's head is placed in a stabilizing frame to prevent movement during treatment, and other steps are undertaken to ensure safety. Following the identification of the target region for ablation, ultrasound is applied in incremental units of increasing intensity known as sonications while MR thermometry provides real-time information about the temperature at the target site. Following each sonication, the patient and physician evaluate the reduction in tremor. Treatment continues until a satisfactory result is achieved. Following the procedure, patients are typically observed for a short time and then go home. Unlike invasive surgical procedures, MRgFUS allows patients to return to daily activities within a day or so of the procedure.
Clinical Studies of MRgFUS in ET
Numerous clinical trials have been performed to investigate the safety and efficacy of MRgFUS, and the procedure's effect on quality of life (QOL). In general, meta-analyses of these trials suggest that MR image-guided focused ultrasound thalamotomy offers substantial improvement in hand tremor scores, Clinical Rating Scale for Tremor (CRST) scores, and Quality of Life scores.
FDA approval for MRgFUS treatment of ET was based on its pivotal study, a prospective, double-blind, randomized, controlled trial of MRgFUS for unilateral thalamic ablation in ET. In this trial, the primary endpoint, CRST at 3 months, was significantly improved in the MRgFUS group (p<0.001). Secondary outcome measures, including disability and quality of life, were also significantly improved. However, persistent adverse neurologic effects at 12 months, including gait disturbance and paresthesia, and the absence of longer-term efficacy findings, were issues. [1] These concerns were addressed in follow-up studies at three and five years.
Among the 67 patients who took part in the open-label extension phase of the study, improvement in tremor score from baseline was durable at two years (56%). The disability score at baseline (which improved by 64% at six months) was sustained at 3 years. [2]
A further analysis of this trial at 5 years post-treatment found similar evidence of durable efficacy. Among the 40 patients evaluable at five-years, CRST scores for postural tremor in the treated hand remained significantly improved by 73.1% from baseline, and combined hand tremor/motor scores improved by 40.4%. Functional disability scores remained improved through the five-year period despite a slight increase over time (all p<0.0001). Quality of Life in Essential Tremor Questionnaire (QUEST) scores also remained significantly improved from baseline (p<0.0003). All previously reported AEs remained mild or moderate, and no new AEs were reported. [3]
References
- Elias WJ, Lipsman N, Ondo WG, et al. A randomized trial of focused ultrasound thalamotomy for essential tremor. N Engl J Med 2016;375:730-739.
- Halpern CH, Santini V, Lipsman N, et al. Three-year follow-up of prospective trial of focused ultrasound thalamotomy for essential tremor. Neurology 2019;93:e2284-e2293.
- Cosgrove GR, Lipsman N, Lozano AM, et al. Magnetic resonance imaging-guided focused ultrasound thalamotomy for essential tremor: 5-year follow-up results, J Neurosurg 2022;Aug 5;1-6.doi: 10.3171/2022.6.JNS212483.
Case Study

Mr. M, a 78-year old man with a 50-year history of essential tremor affecting his upper extremities, was referred to Penn Neurosurgery in early 2022 by a community neurologist in light of the recent debilitating effect of the tremors on his quality of life.
At presentation, Mr. M reported a positive family history of essential tremor, and that the tremor no longer responded to alcohol as it once had. Over the previous 1.5 years, his tremors had significantly worsened, particularly when eating, drinking, or buttoning clothes. It was at this point that he felt that his tremor was "completely out of control."
Mr. M's previous treatments for ET included primidone with minimal improvement in symptoms, and propranolol, which resulted in significant symptomatic hypotension while on therapy. He has not experienced any cognitive symptoms and does not have any tremor at rest or slowness of movement that would suggest Parkinson's disease or another movement disorder. He is, moreover, neurologically intact aside from severe tremor. His clinical rating scale score was 56 out of a maximum score of 144. Bilateral upper extremity tremors were noted to have amplitudes greater than 20cm.
At Penn Neurosurgery, Mr. M discussed deep brain stimulation and focused ultrasound with neurosurgeon Iahn Cajigas, MD, PhD, who initially recommended deep brain stimulation, given the bilateral nature of Mr. M's tremor (MRgFUS was not indicated for bilateral application at the time of Mr. M's treatment). Mr. M declined to consider this more invasive option, however, and opted to receive instead a left thalamotomy with focused ultrasound for control of his dominant right hand tremor.
On the morning of Mr. M's procedure, his head was shaved to accommodate the physics of ultrasound travel through air versus brain tissue and allow more efficient transfer of energy into the brain. His head was then placed within a special frame that provides a coordinate system for targeting areas within the brain.
After a brief amount of local and intravenous anesthesia for the frame placement, Mr. M was brought into the MRI treatment room. There, he completed a spiral test for Dr. Cajigas, to serve as baseline for the treatment response (Figure 1A). Low energy sonications were then performed to confirm device function and targeting accuracy. Between each sonication, Mr. M was examined to ensure the absence of any side effects, such as weakness or numbness. Once precise energy delivery was confirmed, a total of two higher energy sonications at treatment temperatures were performed.
Following his treatment, Mr. M completed a spiral test to demonstrate his response to treatment (Figure 1B). Overall, there was an approximately 95% reduction in tremor amplitude.
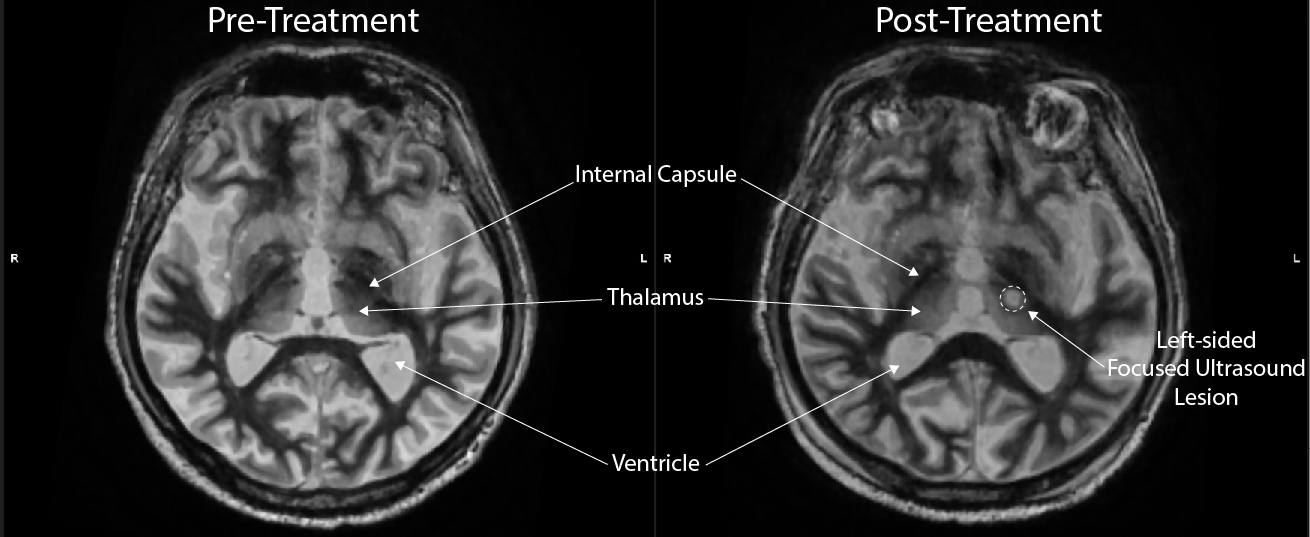
After treatment, the Mr M had a physical therapy evaluation and was discharged home in the early afternoon. A post-treatment MRI performed prior to discharge (Figure 2) confirmed a lesion within the ventral intermediate nucleus of the thalamus. Immediately prior to discharge, Mr. M was able to eat a cup of soup by raising a spoon to his mouth – something he had been unable to do because of his tremor for many years.
Because Mr. M was treated before the second FDA-approved indication for MRgFUS in ET, he is now a potential candidate for treatment of his left-hand tremor pending further clarification of the risk profile for individuals receiving such therapy.
Faculty Team
Penn neurosurgeons have made inestimable contributions to the field of functional and restorative neurosurgery, having contributed to the latest indication for bilateral focused ultrasound in essential tremor, and to critical investigations in deep brain stimulation (DBS).
Providing Focused Ultrasound Therapy for the Treatment of Essential Tremor at Penn Medicine
Neurosurgery
Access
Penn Neurosurgery
Pennsylvania Hospital
Spruce Building, 3rd Floor
801 Spruce Street
Philadelphia, PA 19107
