

Orthopaedic surgeons at Penn Medicine are performing periacetabular osteotomy (PAO) surgeries for native hip preservation in adolescents, young adults and adults (generally up to 45 years of age) with dysplasia and other structural hip deformities.
Structural hip deformities affect a large proportion of younger adults who present with symptomatic hip pain in the United States. These conditions are often of congenital, developmental, or traumatic origin, and typically involve morphologic abnormalities of the acetabulum or femur leading to instability and/or impingement, a pathological conflict between the two bones during movement.
The mechanical aberrations identified with structural hip deformity commonly involve dysplasia and femoroacetabular impingement (FAI) and their associated pathologies. Hip pathology can also involve malalignment or rotational deformities of the femur (e.g., issues with femoral torsion), among other anomalies.
Impingement occurs when the proximal femur contacts the acetabulum during range of motion, such as flexion and internal rotation. Impingement is often caused by asphericity of the femoral head (cam type) or over-coverage of the acetabulum (pincer type). With dysplasia, insufficient coverage of the femoral head by the acetabulum can lead to symptomatic instability and early labral and cartilage degeneration. This continuum—from impingement to instability—is an important concept in evaluating younger patients with hip pain.
The tantamount consideration in younger patients with dysplasia and/or FAI is to preserve the native hip by addressing underlying structural abnormalities. Accordingly, orthopaedic surgeons at Penn Medicine employ a spectrum of corrective hip preservation surgeries for this population, including both arthroscopic and open techniques.
Periacetabular osteotomy (PAO), for example, addresses the underlying structural deficiencies of a shallow or poorly oriented acetabulum. In PAO, a series of osteotomy cuts encompass the acetabulum, preserving the hip abductors and the posterior, weightbearing column of the pelvis. The socket is then freed from the pelvis and reoriented in a position of better coverage of the femoral head. This offers the opportunity to restore both normal hip joint mechanics and ideal loading of the articular cartilage. The goal is long-term durability of the native joint in adolescent and young adult patients with dysplasia.
PAO is not a “standard” surgery, and patient selection is important. The procedure is demanding, in that osteotomy and precise reorientation are required, and each step requires a certain level of experience and training. However, the potential advantages of PAO, which include greater long-term joint stability and durability of the cartilage, may help younger patients to avoid or delay joint replacement surgery, such as total hip arthroplasty.
Case Study
Mr. J, a 25-year-old man, was referred to the Penn Hip Preservation Center with structural deformity of the right hip, the result of a segmental fracture of the proximal femur at age four. His hip and leg were placed in a cast, and his fracture healed in a malaligned position. As a young adult, Mr. J had chronic, progressive and disabling pain (especially in the setting of his high-demand work as a manual laborer) that he managed with daily opioid medications. In the months prior to evaluation at Penn, he had extensive physical therapy and an intra-articular injection for pain control. He was unemployed for much of this time.
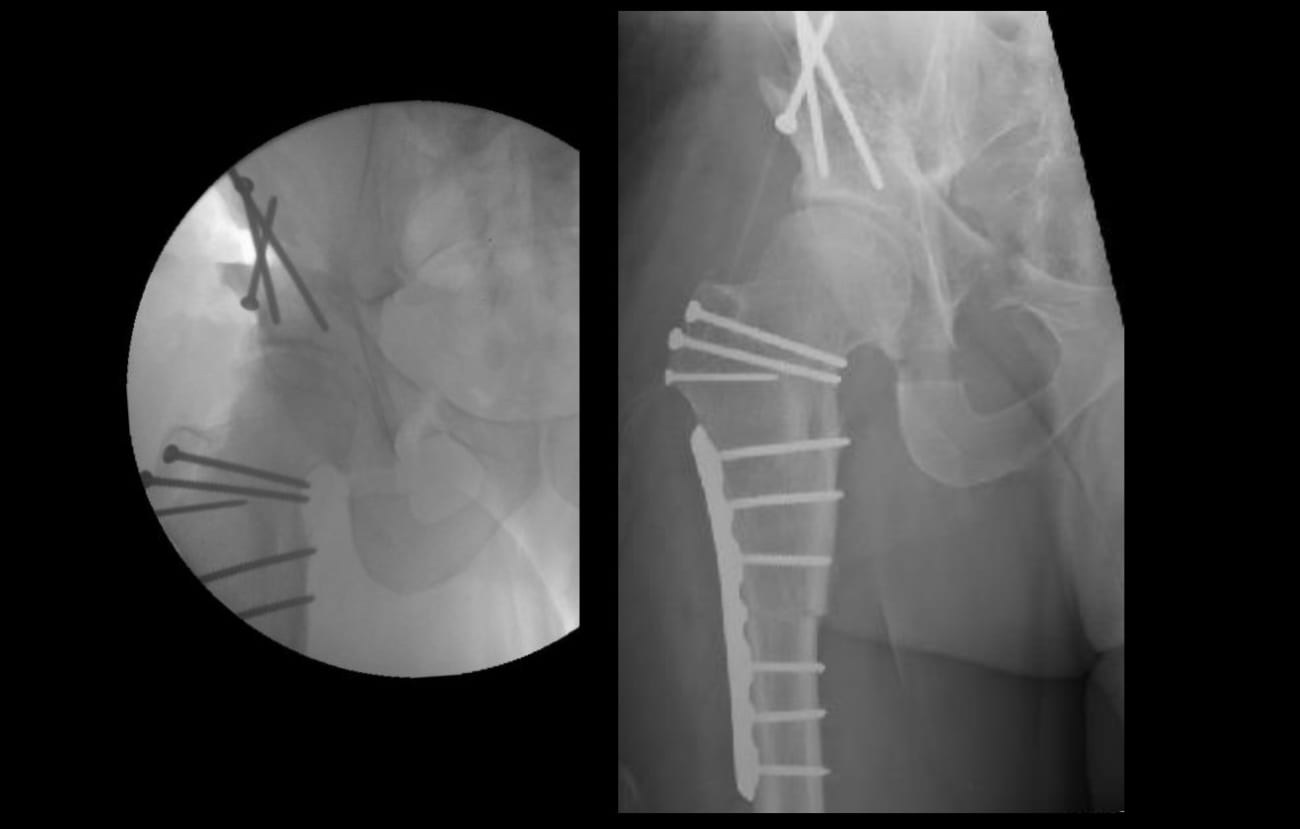
At Penn, Mr. J was deemed a candidate for hip preservation. Imaging determined that he had severe acetabular dysplasia, a tear of his acetabular labrum, a torsional deformity of the femur (45 degrees of retrotorsion) and FAI due to a cam lesion of the femoral head-neck junction (Fig. 1). Despite these abnormalities, however, there was no evidence of overt osteoarthritis at his hip. After discussion of the risks, benefits and treatment alternatives, Mr. J elected to have corrective surgery. Pre-procedural imaging and modeling were completed to ensure proper intra-operative alignment targets of the reoriented hip and femur.
A PAO was performed to correct the acetabular dysplasia. Nerve monitoring and fluoroscopic imaging were used to ensure safe and accurate surgery. Bone grafting was completed at the acetabular osteotomy sites, with autograft harvested from the pelvic osteotomy mobile fragment. A surgical hip dislocation was also performed, with careful preservation of the critical blood supply to the femoral head. To address the intra-articular sequelae of FAI, a labral repair and femoral head-neck osteochondroplasty were completed.
Although Mr. J’s intra-articular causes of FAI were optimized, the extra-articular rotational deformity of the femur did not allow for adequate impingement-free range of motion. Therefore, a subtrochanteric derotational osteotomy with internal fixation was performed to bring the femur into normal rotational alignment. Bone autograft harvested from the greater trochanteric bed was used to supplement the osteotomy fixation (Fig. 2).
Mr. J was on crutches the day after his procedure and was in the hospital for three days, where he received physical therapy, as well as a continuous passive motion machine. Partial weight-bearing was permitted on discharge. He was weaned from all pain medications by several months post-operatively. At six months, he was walking with no gait aids, and by seven months he had found full-time work.
